Imagine you’re the CEO at a reputable healthcare facility. One morning, a routine audit reveals that a long-standing vendor, responsible for supplying essential medical equipment, has been on the List of Excluded Individuals and Entities (LEIE) for over a year. The discovery is shocking; not because anyone acted maliciously, but because the oversight was so simple.
This vendor had been reliable, their products top-notch, and their invoices always matched the deliveries. But now, the facility faces steep penalties, and the trust within the administrative team is shaken.
Exclusion screening isn’t necessarily difficult, but it’s often misunderstood, sidelined, or handled inconsistently.
The good news: it’s entirely preventable.
The better news: it doesn’t have to be burdensome.
What Can Make Screening Seem Complicated?
The Office of Inspector General (OIG) maintains the List of Excluded Individuals and Entities (LEIE): a database of people and organizations banned from participating in federally funded healthcare programs. This includes Medicare, Medicaid, and others.
If your organization hires or works with someone on the exclusion list, and their work is paid for directly or indirectly by a federal healthcare program, that puts the organization at risk. It doesn’t only apply to people who submit claims. It includes anyone, contracted or employed, whose work supports reimbursed services, such as:
- Physicians
- Registered or Advanced Practice Nurses
- Medical Suppliers
- Third-party billing companies
- Temp workers and outsourced staff
- Administrative and executive staff
Organizations have faced penalties not because they intentionally broke the rules, but because someone didn’t get screened when they should have. It might have been a role people didn’t realize needed screening, or a vendor that was assumed to be low risk. Either way, it leads to the same outcome.
To complicate matters more, the OIG doesn’t require organizations to do sanction screening on a specific schedule. In its 2013 Special Advisory Bulletin, it simply states that providers should screen employees and contractors “periodically,” without defining what that means. There’s no set schedule, no template, and no checklist for how to handle vendors or temporary staff. You’re expected to figure it out…and if you get it wrong, you’re still responsible. That kind of ambiguity makes it easy to miss something, and the lack of clear guidance makes it hard to know what actually needs to happen.
Why Vendors Get Missed
Vendors often fall outside normal sanction screening workflows. They do not go through HR, so they rarely get checked against the LEIE.
Not all vendors need to be screened, but if they provide services tied to federal reimbursement such as billing, consulting, or medical equipment, they do. The OIG does not give a list, so it is up to the organization to determine who qualifies.
What Happens If You Miss Someone
If your organization hires or contracts with someone on the exclusion list, and that person provides any service tied to a federally funded healthcare program, the penalties are serious. The government can demand repayment for any claims linked to that individual, even if those claims were otherwise valid.
In many cases, that also comes with civil monetary penalties. The OIG can fine organizations up to $20,000 for each item or service provided by an excluded person. On top of that, they can add an assessment of up to three times the amount claimed. These penalties apply whether the excluded person was hired directly or worked through a third party.
The OIG will not ask whether it was intentional. It does not matter if the work was non-clinical. If the person was excluded and connected to federal reimbursement in any way, the organization is held responsible. That is why the screening process has to be both broad and consistent. It is not just about avoiding penalties. It is about knowing you are not taking that risk in the first place.
If You Find Out Too Late
Mistakes happen. Someone might get missed during onboarding, a name might not match exactly, or a contractor might bypass the usual process. If you find out that you have hired or worked with someone on the exclusion list, the most important thing is to act immediately.
Start by removing the person from any work connected to federally funded healthcare programs and document everything:
- When you discovered the issue
- What their role was
- How the oversight happened
- What steps you took in response
You should also assess whether any claims submitted during their time with your organization are tied to federal reimbursement. If they are, consider reporting the issue through the OIG’s Health Care Fraud Self-Disclosure. This process gives organizations a way to report potential violations before they are discovered during an audit or investigation and shows that they are taking responsibility instead of trying to avoid it. In many cases, it can be the difference between a manageable resolution and something far more serious.
Delaying the response increases the risk. The sooner you act, the better positioned you are to contain the issue and prevent it from growing into something larger.
Final Thoughts
Exclusion screening is one of those things that looks simple until you actually have to manage it. The rules leave room for interpretation, but the consequences do not. You are responsible for catching people who shouldn’t be working with your organization, even if the process to do that is unclear or inconsistent.
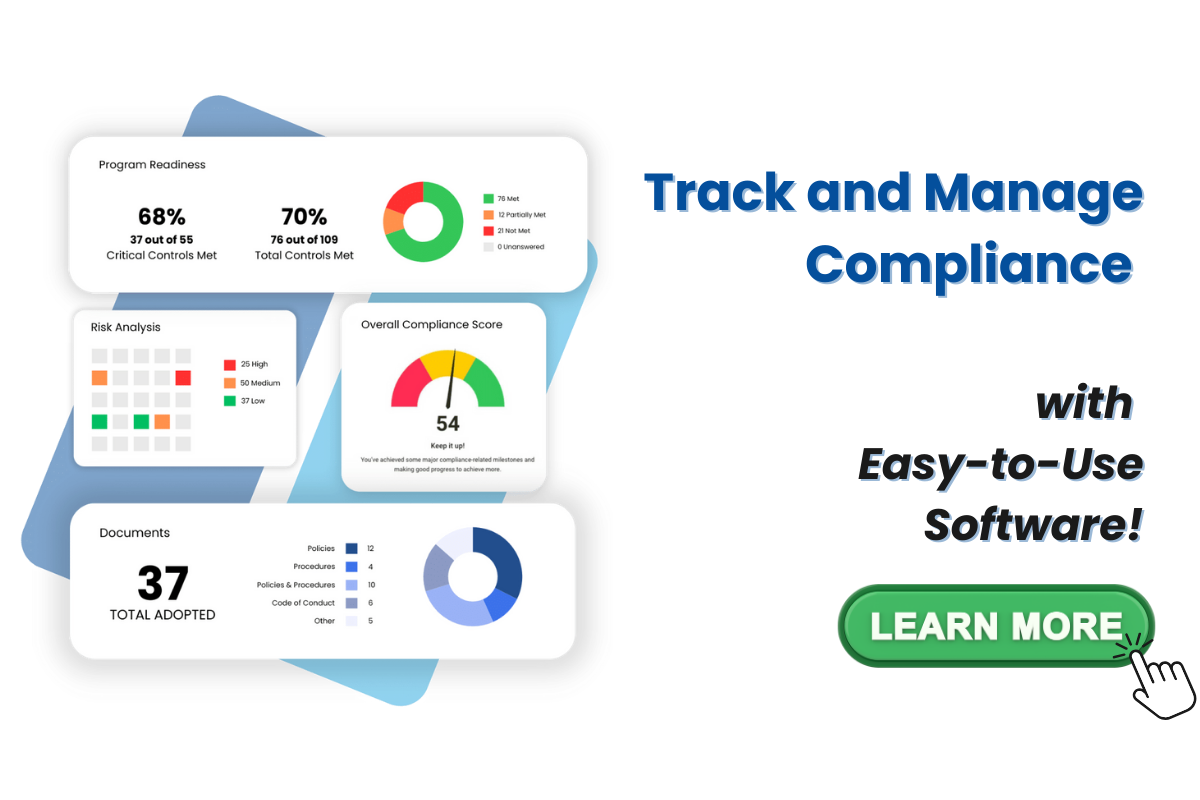
This is where structure matters. Compliancy Group’s Exclusion Monitoring Tool is an exclusion screening software that helps build that structure into your workflow. It checks employees and vendors weekly against 55 exclusion lists, including the OIG LEIE, SAM, and FDA. It links directly to your HR system so your screening list stays current, and it keeps documentation organized in one place.